In Spring 2022, the NHS England Elective Care Improvement Support Team (IST) undertook a qualitative diagnostic review of Walsall Healthcare NHS Trust’s (WHNT) outpatient booking processes, making 19 recommendations for the Trust in their final report.
Keen to address the recommendations made, WHNT embarked on a transformative programme, guided by the IST and their mission was clear:
– Overhaul outpatient booking processes
– Combat high Did Not Attend (DNA) rates
– Optimise clinic utilisation
– Ensure equitable access to healthcare in a region struggling with health inequalities
The Trust put in place an improvement plan and requested support from Four Eyes Insight (FEI) to deliver tangible improvements against the most challenging areas of reducing DNAs, improving clinic utilisation, improving governance, and providing training.
At its core, the programme was scoped to support WHNT to address health inequalities, and improve patient access to the Trust and was part of a wider package of work underway to reduce safety risks associated with long waits.
The patient population served by the Trust is characterised by its diversity in terms of socio-economic status, introducing unique challenges related to digital disparities, language barriers, and financial constraints. WHNT is in the 10% most deprived districts in the country, and its population experiences significant health inequalities; with both infant and under-75 mortality from preventable causes significantly worse than the England average, with the COVID pandemic exacerbating existing issues across the region.
Target KPIs
The programme launched with an Insight and Discovery Phase, used to identify opportunities and agree on stretching yet realistic key performance indicators (KPIs) on which the programme’s success could be measured. The KPIs encompassed both numerical metrics and process-driven initiatives, representing a holistic approach aimed at demonstrating tangible outcomes and ensuring the sustained effectiveness of the interventions. KPIs included:
- – Achieving a 2% increase in booked and capacity utilisation
- – Achieving a 2% reduction in the DNA rate
- – Tangible evidence of an increase in patient attendance
- – The implementation of a refined 642 booking process
- – Impact scoring of Admin and Clerical training
- – Tailored DNA reduction initiatives within agreed specialties
- – The establishment of streamlined communication channels
A collaborative ethos that ensured both FEI and WHNT were fully aligned with the programme’s objectives was a critical component of the programme’s success. Other crucial contributing factors to the realisation of the KPIs included:
1: Establishing a robust governance structure to underpin the programme’s delivery
2: Develop a comprehensive set of reports to baseline and track performance
3: Creating a patient-centric approach with special attention given to traditionally under-represented demographics, ensuring that the programme was finely tuned to address patient needs and concerns.
Adopting a phased approach enabled quick implementation of improvements and offered agility to adapt and fine-tune the new processes at pace. The four core phases were:
1: Insight and discovery:
Engagements, onsite observations, and data analysis led to KPI development.
2: Implementation of process change:
Guided by the results of patient feedback, the multidisciplinary Task-and-Finish Groups supported two core workstreams to agree upon and implement new processes.
3: Delivery period:
At the time of physical change, KPIs were closely monitored to measure the impact.
4: Handover:
With assurance, the results could be sustained.
The programme encompassed a range of process changes that were implemented to address specific challenges the Trust faced. The result was a tangible improvement to operational delivery, providing healthcare professionals with more structure and visibility in business-as-usual tasks. For patients, the work has improved access to healthcare, increased available slots, and provided a range of communication methodologies that were previously unavailable.
Increasing Utilisation
Specifically, the core actions taken to enable an increase in utilisation are as follows:
-
- Vacant Slot Report (VSR): FEI collaborated with the health informatics team to create an hourly-refreshing VSR, offering a real-time view of available capacity. This data empowered better capacity utilisation.
- Slot Management Rules: Rules were developed to guide staff on converting and managing short-notice capacity efficiently.
- Digital Solutions for Patient Communication: Introducing enhanced patient communication methods enabled rapid notifications to multiple patients regarding short-notice appointment capacity. This approach significantly reduced the time required to fill open slots compared to traditional phone call-based scheduling, increasing utilisation of capacity and releasing staff to focus on scheduling up to 6 weeks in advance.
- Addressing Recurring Capacity Gaps: FEI identified and resolved chronic underutilisation issues by collaborating with clinical and operational leaders. Solutions included template changes, adjusted booking rules, and the release of reserved slots to optimise utilisation.
- 642 Process Enhancement: The programme revamped outpatient estate and clinic utilisation management. We refined 642 scheduling meetings with a new Standard Operating Procedure focused on forward planning and action, supported by an interactive floor plan amongst other tools for better visibility of capacity.
- Streamlined Communication Channels: The introduction of a centralised area on Microsoft Teams established a clear structure for efficient outpatient and communication operations. The Trust began to utilise a RACI matrix for escalation policies to ensure communication reaches the right recipients at the right time and we designed Microsoft Forms for streamlined short-notice booking requests, improving clarity.
Reducing DNAs
In order to reduce DNAs, several steps were taken to modify processes such that disadvantaged patient populations would not be disproportionately affected. The critical changes embedded included:
-
- Appointment Reminders: Rolled out to over 200 previously excluded clinics, with voice reminders being introduced for patients without mobile phones and efforts made to provide reminders in multiple languages.
- Transport Support: Following a pilot project assessing the impact of offering free transport options to patients, a streamlined process for claiming travel costs was introduced. Patients could now be reimbursed on the day of the appointment, eliminating the need for lengthy processing. Information sheets explaining the process and eligibility were included with appointment letters, resulting in increased financial support uptake and helping to reduce DNA rates.
- Letter Enhancement: Letter language was simplified, and patients were encouraged to check in at the outpatient reception desk to receive directions once at the hospital.
- Webpage Translation: A dedicated webpage was created to translate appointment reminders into different languages, ensuring inclusivity for patients with diverse linguistic backgrounds and enabling automatic translation during phone calls with hospital staff.
- Printing Letters: Issues related to letter communication were addressed, including ensuring all users could print externally for timely letter delivery. Training materials were provided to support appointment booking.
- Bespoke Processes: Specialty operational and clinical leads collaborated to develop targeted approaches where DNA rates were high; including, overbooking slots in some clinics, implementing Patient Initiated Follow-Ups (PIFU), and using bespoke text messages to address specific challenges in various specialties.
- Validation Initiatives: Validation exercises initiated in specific specialties, like Gynaecology and Trauma and Orthopaedics, expanded across the Trust. FEI drafted Standard Operating Procedures (SOPs) which the Trust rolled out across specialties.
Patient-Centric Results
The actions mentioned in the previous section enhanced healthcare resource management, patient engagement, clinic operations, and communication efficiency.
As a result of these actions, the following tangible improvements were realised:
– 4.8% improvement in Booked Utilisation
– 3.1% improvement in Capacity Utilisation
– An increase of 1255 attendees across the 6-week delivery period
– Reduction of 52 DNAs per week
– 14% reduction in patient complaints
In addition, the Trust has seen £1.73M ERF income for the first 5 months of the year attributed to outpatient attendances and a £9000 reduction in monthly outpatient WLI spend.
“Working alongside Walsall to deliver this programme has been a very rewarding experience. Together, we have improved the operational processes within the outpatient department, leading to better use of the available capacity, easier communication routes for patients, and a marked reduction in the volume of patients who have missed their appointments. The success of this programme can in part be attributed to the dedicated time the Trust has provided to drive forward the changes alongside us. Despite significant operational pressures, the end goal has remained a firm focus and Trust colleagues have embraced the capacity and subject matter expertise our support provides.”
Samantha Sullivan,
Delivery Director,
FEI.
To learn more about how Four Eyes Insight can help your Trust improve, contact us through the button below.
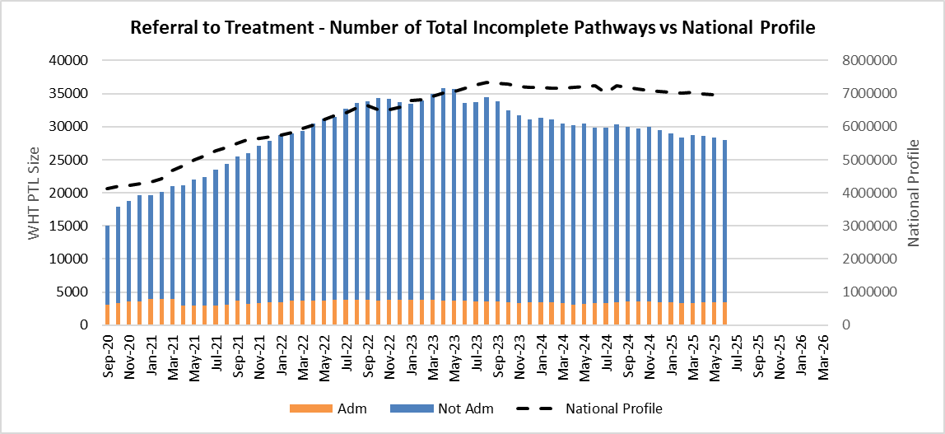
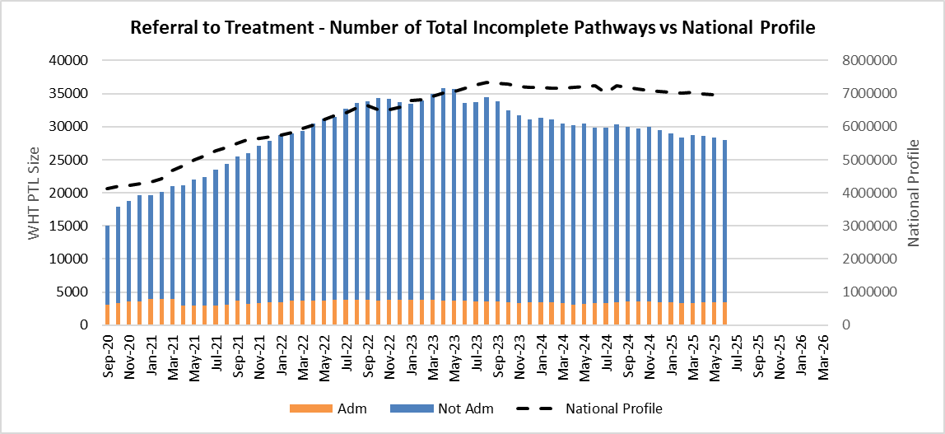
Two years on: Sustained Improvement
Two years on from programme delivery, Walsall has sustained the rigour and governance established during the programme. As of July 25, booked utilisation stands at 95%, and the non-admitted waiting list continues to decline.
The graph below illustrates the Trust’s position in comparison to the national profile:
Connect with Samantha on LinkedIn.
In partnership with Walsall Healthcare NHS Trust, we’ve been shortlisted for the 2024 HSJ Partnership Awards in the category of Best Elective Care Recovery Initiative.